Microcystic Adnexal Carcinoma (MAC) may not be as well-known as some other skin cancers, but its unique characteristics and potential impact on health make it a topic worth exploring. In this post, we’ll delve into what MAC is, who is susceptible to it, its appearance, treatment options, prognosis, and survival rates.
What is Microcystic Adnexal Carcinoma?
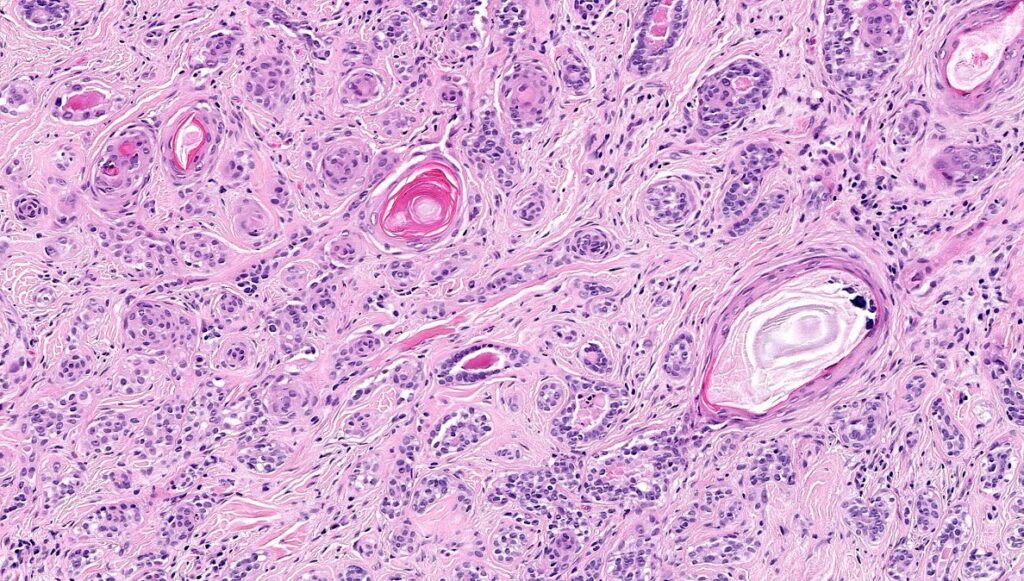
“Microcystic Adnexal Carcinoma is a rare and slow-growing type of skin cancer that originates in the sweat glands and hair follicles,” explains Dr. Adam Mamelak, board-certified Dermatologist and Mohs surgeon. It typically presents as a painless, firm, flesh-colored or slightly yellowish nodule or plaque on the skin. MAC tends to infiltrate surrounding tissues and nerves, making complete surgical removal challenging.
Who Gets Microcystic Adnexal Carcinoma?
MAC predominantly affects adults, typically between the ages of 40 and 70 years old. While it can occur in individuals of any race or ethnicity, some studies suggest a slightly higher prevalence among Caucasians. There is no clear gender predilection for MAC.
What Does Microcystic Adnexal Carcinoma Look Like?
Microcystic Adnexal Carcinoma often appears as a small, indurated, skin-colored or slightly yellowish papule or plaque on the face, particularly in the nasolabial fold or periorbital region. The lesion may have a smooth or slightly waxy surface and may be mistaken for benign skin conditions such as sebaceous hyperplasia or basal cell carcinoma.
How is Microcystic Adnexal Carcinoma Treated?
Treatment for Microcystic Adnexal Carcinoma typically involves surgical excision to remove the tumor with clear margins of healthy tissue. Due to the infiltrative nature of MAC, achieving complete removal can be challenging, and recurrence rates are relatively high. “Mohs micrographic surgery, which allows for precise microscopic examination of tissue margins during surgery, is often recommended to minimize the risk of recurrence,” says Dr. Mamelak.
Prognosis and Survival Rates:
The prognosis for Microcystic Adnexal Carcinoma is generally favorable with appropriate treatment. However, due to its infiltrative growth pattern and potential for local recurrence, long-term surveillance is necessary. The risk of metastasis is low, but MAC can cause significant morbidity if not adequately treated.
Conclusion:
While Microcystic Adnexal Carcinoma is rare, its potential impact on health underscores the importance of early detection and prompt treatment. Understanding the risk factors, symptoms, and treatment options can empower individuals to seek timely medical attention and advocate for their health. By raising awareness and promoting regular skin examinations, we can work towards improving outcomes for those affected by this rare but impactful skin cancer.